How long does bone healing take?
Bone generally takes 6-12 weeks to heal. This does depend on the location and severity of the fracture however, with more complex fractures of bigger bones taking longer than 3 months.
Recovery from a fracture can also take longer than this, due to the impact on the surrounding structures. For example, if you fracture your tibia (bone in lower leg), you may be put into a cast and told not to weight bear until the fracture has healed. You will then develop stiff joints and weaker muscles.
Other factors can influence the healing times of bone.
What can hinder bone healing?
Many factors can influence how quickly bones takes to heal. These include:
- Advancing age (we heal slower as we get older)
- Medications (corticosteroids and immunosuppresants)
- Medical conditions (diabetes, hormone=-related problems, vascular diseases)
- Smoking (constricts blood vessels, reducing circulation of blood)
- Poor nutrition or poor sleep
- Low levels of calcium or vitamin D
Movement of bone fragments can also negatively affect healing, which is why fractures are sometimes put into a cast and weight-bearing is prevented.
However, weight-bearing/loading bones is also key to growth and production of new bone and therefore following a healthcare professionals advice is important to know when and how much to weight-bear.
How do bones heal?
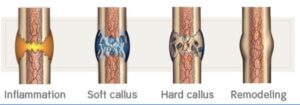
Fractures/breaks to bones all undergo the same process of healing. This process has three overlapping stages:
- Inflammation (several days)
- Bone production (several weeks)
- Bone remodelling (several months)
See below for these stages in more detail.
Inflammation (0-2 weeks):
Haematoma formation starts immediately after the bone is fractured and is closely followed by inflammation which lasts for several days. A haematoma is a collection of blood outside of the blood vessels (bruise).
The bleeding around the bone site leads to inflammation and clotting of blood at the fracture site. This provides the initial structural stability for producing new bone.
Bone production:
This can be broken down into 2 stages. Soft callus formation (2-3 weeks) and hard callus formation (3-6 weeks)
The clotted blood formed by inflammation is replaced with fibrous tissue and cartilage (soft callus). This is replaced with hard bone (hard callus) as the healing progresses.
Bone remodelling (8 weeks-2 years):
Bone remodelling is the final phase of bone healing, and can continue for many months. As the bone continues to form, it becomes compact and returns to its original shape. Blood circulation also improves to the area. In this phase, weight-bearing is more beneficial as there would have been adequate bone healing, and the weight on the bone helps to encourage bone remodelling.
During the process of bone healing, altered behaviours and movement patterns are likely to have occurred. Also, muscle wasting around the area is likely due to less impact/weight going through the body. This is where Physiotherapy plays a key role in rehabilitation.
Through strength and conditioning, an individualised exercise programme can be created, aimed at restoring the body to its previous level of function, and returning the individual to their normal activities.
GTPS (Greater trochanter Pain Syndrome) is an umbrella term that encompasses conditions that result in pain in the outside of your hip. Other names for this include trochanteric bursitis or gluteal tendinopathy and it is due to injury, irritation or inflammation to the tissues that surround the outside of your hip.
Symptoms
- Pain in the outside of the hip
- Worse with activities such as running, standing or walking
- Tender to touch
- Pain when crossing the leg over your body
- Pain when lying on that side.
This is a common condition that we see in runners and there can be various factors that lead to this pain occurring.
Typically, it is related to overloading the tendons of the hip or increasing training too rapidly.
Hip pain can also be referred from the back.
Tips
- Avoid crossing your legs until the symptoms settle, using a pillow between your knees at night
- Adjust your running style or consider your footwear
- Strengthen the hip
See a Physiotherapist at Hallamshire Physiotherapy for a thorough assessment, to determine the factors influencing the pain and how to manage/treat and avoid the pain from returning.
See New ‘Physio Clinic’ Q&A session (ukbouldering.com) for a previous thread of Q&As with our Physiotherapy team covering various cases.
Stress incontinence in men is the most common form of urinary incontinence. Stress incontinence occurs when urine accidentally leaks when you cough, sneeze or laugh. Physiotherapy with Hallamshire Physiotherapy Clinic can help to significantly to reduce symptoms that are associated with stress incontinence.
What is Stress incontinence?
Urine is constantly travelling from your kidneys and is collected in your bladder. Your bladder then expands as it fills with urine. The bladder is a muscle and is kept closed by a valve called the sphincter until the bladder becomes full. When the bladder is full, the sphincter opens and urine is taken via a tube called the urethra to be passed.
Stress incontinence in men is when urine accidentally leaks due to a sudden increase in pressure or stress on the bladder, sphincter and urethra. This can occur in incidences such as sudden laughing, coughing or sneezing.
What causes stress incontinence in men?
Stress incontinence in men is caused by weakness of the pelvic floor muscles so that these muscles, the bladder, sphincter and urethra cannot withstand any extra pressure or stress. The extra pressure in the abdomen means that the sphincter has difficulty staying closed and urine is leaked. The amount of urine that is leaked may vary and can either be a small or large quantity.
Stress incontinence in men can be caused by a number of reasons that result in weakening of the pelvic floor muscles.
- It can be caused by any disease, condition or injury that results in damage to the nerves that activate the muscles in the pelvic area. Diabetes, Parkinsons, stroke, spinal cord injuries and other neurological conditions are likely to cause decreased bladder control. The prostate gland surrounds the urethra and is responsible for producing semen
- Problems with the prostate such as prostate cancer or enlargement of the prostate can cause decreased bladder control. Also, surgery of the prostate can result in significant weakening of the pelvic floor muscles and therefore bladder problems.
Symptoms:
Stress incontinence in men causes symptoms such as leaking of urine when you:
- Cough, laugh or sneeze
- Exercise (particularly jumping)
- Lift or do any movement that puts pressure on the bladder e.g. bending
- During sex.
Physiotherapy
If you suffer from stress incontinence then we will work with you in a physiotherapy programme that will include treatment methods which focus on minimising the problems that you are experiencing. Treatment methods include:
- Strengthening exercises for the pelvic floor muscles and abdominal muscles
- Bladder training to help the bladder return to normal function
- Electrical stimulation may also be used to improve muscle function
- Instruction and provision of a home exercise programme to improve pelvic floor function
- Instructions on how to control pelvic floor and abdominal muscles during coughing, sneezing and laughing etc.
- Breathing control and relaxation exercises
- Education on how to make lifestyle changes that may affect the bladder.
Vulvodynia is persistent, unexplained pain in the vulva. The vulva is the female genital area including the skin surrounding the opening of the vagina.
It can happen to women of all ages. Vulvodynia can become a long-term problem that’s very distressing to live with, but much can be done to help relieve the pain.
Symptoms of vulvodynia
The main symptom is persistent pain in and around the vulva and vagina. The vulva usually looks normal.
The pain may be:
- Burning, stinging, throbbing or sore
- Triggered by touch, such as during sex or when inserting a tampon
- Constantly in the background
- Worse when sitting down
- Limited to part of the vulva, such as the opening of the vagina
- More widespread – sometimes it can spread over the whole genital area and the anus.
Some women also have problems such as vaginismus (where the muscles around the vagina tighten involuntarily), interstitial cystitis (a painful bladder condition), painful periods and irritable bowel syndrome (IBS).
Having persistent vulval pain can affect relationships, reduce sex drive, and cause low mood and depression.
Pain in the genital area is often embarrassing to talk about and can make you feel isolated.
Things you can do to help with vulvodynia
If pain persists you can seek advice from the GP and/or Physiotherapists however there are lifestyle changes may help reduce symptoms:
- Wear cotton underwear and loose-fitting skirts or trousers
- Avoid scented hygiene products, such as feminine wipes, bubble bath and soap (an emollient is a good substitute for soap)
- Apply cool gel packs to your vulva to soothe the pain
- Use petroleum jelly before swimming to protect the vulva from chlorine
- Try not to avoid sex or touching your vulva completely, as this may make your vulva more sensitive. If sex is painful, try to find a position that’s more comfortable, or do other sexually intimate activities together until you have sought advice if penetration is painful
- Try to reduce stress, as it can increase the pain of vulvodynia
- For pain when sitting, using a doughnut-shaped cushion can help.
Physiotherapy
A physiotherapist can teach you some pelvic floor exercises (such as squeezing and releasing your pelvic floor muscles) to help relax the muscles around your vagina.
Another technique to relax the muscles in the vagina and desensitise it involves using vaginal trainers. These are smooth cones of gradually increasing size and length that can be inserted into your vagina in the privacy of your own home.
Some physiotherapists may also suggest trying TENS (transcutaneous electrical nerve stimulation) to reduce your pain. This is where a machine is used to deliver a mild electrical current to the painful area.
Urinary incontinence can be devastating. Here are some facts:
- Millions of people in the UK suffer from incontinence
- It can affect up to one in three women and up to one in ten men
- It affects people of all ages
- Due to the associated embarrassment, it can lead to a number of other mental and emotional health problems (including anxiety, depression and social isolation) not to mention a loss of dignity
- It also leads to urinary tract infections, which can cause confusion and falls in an ageing population, resulting in avoidable hospital admissions
- It is the second main reason why women are admitted into care homes
- It is expensive: incontinence pads or so-called ‘containment products’ are not cheap, and it has huge social and healthcare cost implications for the NHS
- It is often treatable and/or preventable.
Below are descriptions of the main types of incontinence which can affect men and women.
Stress urinary incontinence
Caused by a rise in intra-abdominal pressure (eg. on coughing, sneezing, shouting, laughing, lifting, bending or standing up from sitting).
Urgency and/or urge incontinence (also known as ‘overactive bladder’)
A sudden compelling urge to pass urine, and maybe leaking on the way to the toilet.
Mixed urinary incontinence
A combination of stress urinary incontinence and urge incontinence.
Faecal urgency and/or incontinence
A sudden strong urge to open one’s bowels, and/or not making it to the toilet and losing stool.
Functional incontinence
Where disability, reduced mobility or problems with manual dexterity limit one’s ability to make it to the toilet or to remove clothing in time.
Given the profoundly negative impact it can have on people’s lives, why don’t more people seek help? Evidence suggests that only 20% of women sufferers will be treated actively (and that figure is based on the number of women who actually come forward). Often they think it’s normal (it may be ‘common’ but it’s not ‘normal’) or they blame themselves, for example, for not doing their pelvic floor muscle exercises. (The problem is, often women who do their exercises are doing them incorrectly, as they may only have been given a leaflet telling them what to do.) Or they simply don’t know what their treatment options are. Evidence shows, for example, that two thirds of women who suffer from stress urinary incontinence can be cured by following a course of supervised pelvic floor muscle training. The research is also favourable regarding outcomes for men.
National health guidelines identify physiotherapy as the first-line course of treatment for urinary incontinence. It’s non-invasive and can be highly effective. Yet how many people know what women’s health physiotherapists really do, or how pelvic floor muscle training can help men with bladder problems? Unlike continence nurses, physiotherapists don’t manage ‘incontinence’: the aim of treatment is to get their patients dry. That’s why specialist physiotherapy should consist of a lot more than just pelvic floor muscle training. Ideally it should include bladder re-education, dietary and fluid intake advice and advice on bowel habits and exercise. It should focus on functional use of the pelvic floor muscles to regain bladder control and should educate patients about how to avoid bad habits which weaken or damage the effect of those muscles.
If you would like to discuss any of the above, in confidence, please contact the clinic and speak to Charlotte Pearson.
Around half of all women who become pregnant will develop back or pelvic pain at some point during their pregnancy.
It is very common to get backache or back pain during pregnancy, especially in the early stages. During pregnancy, the ligaments in your body naturally become softer and stretch to prepare you for labour. This can put a strain on the joints of your lower back and pelvis, which can cause back pain.
Pain can be felt in the lower back or buttocks, or over the pubic bone (called Pubic Symphysis Dysfunction). The pain is often worse on one side and may even swap sides from one day to the next.
Pain that comes from the back is often different to pain that comes from the pelvis. Pelvic pain is often misdiagnosed as sciatica and as the treatment for these two conditions is quite different, it is important to have a full assessment from a qualified professional, experienced in the treatment of pelvic pain in pregnancy, in order to decide how to treat the pain.
Pelvic girdle pain ( PGP) is not harmful to your body but it can make it painful for you to get around. Women with PGP may feel pain over the pubic bone, across one or both sides of their lower back, in the area between the vagina and anus or spreading into the thighs. Pain can be worse on walking, going up or down stairs, standing on one leg, turning over in bed or moving legs apart when getting out of a car.
Treatment
Back pain in pregnancy can be treated by protecting yourself and your posture. Physical aids like support belts can also work and can be prescribed by your Physiotherapist.
Pelvic Pain usually occurs when the pelvic joints are ‘unlocked’. Treatment involves learning how to ‘lock out’ your joints during your daily activities to control the pain. A support belt will help to control some of the movement in your pelvis and you will be taught exercises to stabilise your pelvis. Uneven stiffness in your back or hips may also cause the pelvic joints to become over-stressed and mobilisation of these joints will help to reduce symptoms.
Transverse Myelitis is an inflammatory response that causes damage to the spinal cord. This results in varying degrees of weakness, sensory alterations and autonomic dysfunction below the level of the damage.
Transverse myelitis is a rare disorder with approximately 4 new cases per million people per year are diagnosed. It can affect people of all ages however it is most common between 10-19 years and 30-39 years.
The effects of Transverse Myelitis can progress rapidly over minutes or may progress over a period of weeks. The effects seen will be dependent on the level of the spinal cord damage.
There can be a reduction or a complete loss of:
- Sensation
- Voluntary movement
- Proprioception
- Bladder and bowel function
- Sexual function
There could also be issues with
- Reduced ability to breathe deeply and cough
- Pain
- Muscular spasms
Physiotherapy Treatment
The Therapists at Hallamshire Physiotherapy can help you to reach your potential by treating the problems that arise from the diagnosis. Following an assessment you and the therapist will set goals for your rehabilitation.
Physiotherapy includes:
- exercise and stretches
- Joint mobilisation
- Pain control
- Minimising secondary complications
- Provision of orthotics and other equipment
- Advice on handling and positioning techniques
- Teaching transfers and mobility
- Breathing exercises
- Referral to other health professionals
The aim of Physiotherapy is to assist you with in creasing function and independence to lead a fulfilling life.
Optimising your position on the bike will help improve performance and reduce the risk of injuries. Balancing how your body works to the demands of cycling is not straight forward and we too often see the effects of incorrect advice and set up. Don’t delay ring today (tel. 0114 2671223). Our Bike Fit service is provided by Matt Withycombe and Mat Thompson. Ring the clinic to make an appointment or ask to speak to Matt Withycombe for further information that is specific to your needs.
Sheffield has a large cycling population partly due to the close proximity of the Peak District National Park with an abundance of winding country lanes and trails This beautiful area attracts all types of cyclists consisting of leisure/touring, mountain biking, road and triathlon.
The repetitive nature of cycling has the potential to cause problems (click here for link to Matt discussing knee pain in cyclists). When observing the statistics, competitive cyclists average up to 5,000 pedalling revolutions an hour, between 10-150 miles each session and up to 20,000 miles a year. It is therefore easy to understand that even very subtle irregularities with the bike or cyclist can manifest into discomfort and pain and possibly time off the bike.
As specialist physiotherapists at the Hallamshire Physiotherapy Clinic we come into regular contact with cyclists presenting with related and unrelated injuries or problems. The commonest injury prone areas we observe in cyclists are the neck, back and knees.
A cyclists’ flexibility and joint/muscle movement is fundamental to gaining particular positions when riding a bike. This is relevant if you are competing in a time trial where an aerodynamic forward position is required as opposed to a touring cyclist who will require a more comfortable position for longer periods in the saddle.
There can be many reasons for the onset of pain in cyclists. Commonly we observe that the bike set up or “Bike fitting” is incorrect. For instance, if the bike is too big then this can result in overreaching and potentially cause irritations of both the neck and lower back. If the saddle is too high, then a rider will tend to over extend the knee when the pedal is furthest away from them causing excessive pelvis movement from side to side. This again can cause lower back pain as well as pain behind the knee. The list goes on from fitting cleats incorrectly in relation to the pedal spindle, as well asymmetries in hip, knee and foot alignments. Ultimately the bike should fit the rider and not vice versa.
A correct bike fit is paramount and we are offering a new bike fitting service combined with a musculoskeletal screening assessment for cyclists of all abilities aimed at injury prevention.
“Matt Withycombe carried out a road bike fit for me and the adjustments he made have led to a much more comfortable cycling experience, especially on day-long sportives such as the Fred Whitton. Thanks, Matt.”
What does the bike fit service involve?
In brief an initial physical assessment will be undertaken by a physiotherapist to gain an understanding of a cyclists body shape and flexibility. This is followed by an observation of the cyclist pedalling on a static turbo trainer on his/her bicycle. A variety of measurements of the cyclist and the bicycle will be taken throughout the bike fit to enable appropriate adjustments in order to optimise an individuals position relative to the type and level of riding. We are all different shapes and sizes with varying trunk and limb lengths and ultimately the bike should be manipulated to fit the individual cyclist. Minor adjustments can be significant when you think of the repetitive nature of the pedalling action.

More detailed description of each process of the bike fit:
1. Rider and bike information
Initially we need crucial information about the type of riding you undertake i.e. leisure, triathlon, racing or time trial etc. as well as the bicycle you ride and level of experience or expertise. A history of previous injuries or present injuries whether it is related or unrelated to cycling is also very important as physical compensations may have occurred. The type and brand of shoe wear will be needed i.e. road or mountain bike cleats or just normal shoe wear, as this has relevance to the actual bike fitting process.
2. Physiotherapy assessment
Prior to sitting on your bicycle we will need to assess and observe your standing and sitting postures from all directions to gain an understanding of your body shape. A few simple physical tests will also be observed in weight bearing that will give vital information on joint mobility and control. General joint movements and soft tissue flexibility will also be assessed and this is fundamental in identifying any potential problem areas, in particular if you have any previous or present injuries. We basically need to know how you move and your own limitation and asymmetries.
3. Shoe wear
The next phase is to assess the type of shoes you wear for your cycling and if you use cleats, the positioning of these is paramount. The cleat position is fundamental to the pedalling action as this is the interface between the pedal and the shoe and ultimately to your transmission of power. A cleat can be moved from fore to aft in order to get the pedal spindle between the first ( base of big toe) and fifth metatarsal phalangeal joints (base of little toe). The cleats can also be moved from side to side depending on the individuals stance and pelvis/hip width as well as rotated depending on lower limb biomechanics. An incorrect cleat and ultimately foot position can result in inefficiency and potential injuries further up the leg.
4. Anatomical reference points & bike measurements
Prior to the actual observation various bicycle measurements need to be taken to allow a comparison of pre and post bike fitting changes. The cyclist will also have boney landmarks identified at the wrist, elbow, shoulder, hip, knee, ankles and foot to provide reference points when analysing the recording of the pedalling action and position on the bike.
5. Cycling observation
The next stage is the observation of the cyclist on a static turbo trainer from all angles using video recording. This data is then analysed through slow motion and freeze framing with constant referencing to the anatomical markers. The cyclist will need to warm up to get a more accurate observation of a natural pedalling action and once this has occurred individual measurements can occur.
6. Anatomical measurements – back end of the bike
Initially the back end of the bicycle is focused on and the hip, knee and ankle angles at different stages of the pedalling action will be measured through the use of both static measuring devices and dynamic analysis. A virtual and static plumb line will be used to assess the position of the knee in relation to the foot and pedal spindle. If adjustments are needed then this can be undertaken with further analysis of the new positions. This process will continue until optimal angles and positions of the lower limbs are achieved through saddle and cleat adjustments. The observation of lower limb mechanics will then be viewed from the front and rear to again assess any asymmetries or excessive pelvis movement on the saddle.
7. Anatomical measurements – front end of the bike
Once the back end of the bike or ‘engine room’ is sorted out the focus will then be at the front end. The amount of reach in relation to the trunk, neck and upper limb angles will be assessed and measured. Handle bar width in relation to shoulder width needs to be considered as well as the stem length and height of the handle bars. Hand positions on the hoods, bars and drops need to be observed, particularly the cyclists preferred position. If possible corrections will be made but in some instances certain components may need to be changed in order to gain an optimal position.
8. Incorrect bike sizes
In some cases bike sizes may be incorrect or additional components are needed to be purchased. If this occurs then appropriate advice will be given and a brief re-assessment may be needed.
9. Once the bike fit is complete
After a bike fit we recommend at least 2-4 weeks of cycling to get use to a new position and sometimes further corrections are needed if problems occur. As mentioned a bike fit is very individual and depends on many physical and mechanical interactions and variables.
Ring the clinic on 0114 267 1223 to make an appointment, or to ask Matt Withycombe for further information, or to answer specific questions related to your bike-set-up.
Many older adults experience problems with balance and dizziness. People are more likely to have problems with balance as they grow older. In some cases, you can help reduce your risk for certain balance problems, but problems often can start suddenly and without obvious cause.
Problems can be caused by certain medications, balance disorders, or other medical conditions. Balance problems are one reason older people fall. Maintaining good balance as you age and learning about fall prevention can help you get around, stay independent, and carry out daily activities.
We are living in an increasingly ageing population. Not only do people need to stay fit to cope with the changes to the body brought on by the ageing process, but also to ensure they are strong enough to recover from illness or injury. Physiotherapy is fundamental in promoting recovery and the ability to move.

If you have a balance disorder, you might experience symptoms such as:
- Dizziness or vertigo (a spinning sensation)
- Falling or feeling as if you are going to fall
- Staggering when you try to walk
- Lightheadedness, faintness, or a floating sensation
- Blurred vision
- Confusion or disorientation
- Reduced confidence to leave the house.
If this is the case, then it is important that you get checked out and look to start rehabilitation early before it leads to further problems such as falling. Falls can have very serious consequences as we age. See our page on Falls https://www.hallamshirephysiotherapy.com/condition/falls/ for more information.
Here at Hallamshire Physiotherapy, our experienced and knowledgeable physiotherapists will make a full assessment of the person’s ability and they will identify the key factors causing problems for that individual. Physiotherapy will be aimed at improving strength, balance, coordination, flexibility and fitness. They will also assess mobility both in terms of walking, ease of getting onto and off the bed, chair and floor, as well as specific aspects of functional ability a person identifies.
Physiotherapists will also provide advice and education on the benefits of exercise and help to devise individual programmes. All treatment is patient centred with a strong emphasis on problem solving with realistic, achievable solutions.
Our partners Community Wellness Services offer strength and balance classes at our site at 863 Ecclesall Road. https://www.hallamshirephysiotherapy.com/treatments/exercise863/
We also offer online exercise classes for patients who would prefer to work out from the comfort of their own home.
Home visits are also available by request.
Call us on 0114 267 1223 to see how we can help.
Labyrinthitis is an infection of the inner ear, specifically the labyrinth. Vestibular Neuritis is an infection of the vestibular nerve within the inner ear.
Your inner ear is made up of a system of fluid-filled tubes called the labyrinth. This includes your cochlea, which senses sound, and your vestibular system, which senses movement of your head and helps with balance. Your vestibular nerve passes through your inner ear, taking messages to your brain.
Symptoms
Symptoms can start suddenly and can be associated with flu-like symptoms such as a sore throat, runny nose or a fever.
The most common symptoms of Labyrinthitis are:
- Dizziness or spinning sensations (Vertigo)
- Unsteadiness and feeling off balance
- Nausea and vomiting
- Hearing loss, usually in the ear that is infected
- Tinnitus
- The symptoms of Vestibular Neuritis are very similar, but it does not cause hearing loss or tinnitus.
Labyrinthitis and Vestibular Neuritis can affect both adults and children, but they’re most common between the ages of 30 and 60.

Causes
There are various causes for Labyrinthitis and Vestibular Neuritis.
In the majority of cases, they are caused by a viral infection. However, in rarer cases it can be as a result of the following:
- Bacterial infections, usually middle ear infection (otitis media) or meningitis, that spread to your inner ear. These are more common in children than in adults
- Autoimmune conditions affecting your inner ear. This is a less common cause. If you have an autoimmune condition, your immune system mistakenly attacks some of your body’s healthy tissues, causing inflammation and damage
- Damage to your inner ear, due to an underlying disease, such as meningitis, circulatory problems or Ménière’s disease.
How are they treated?
Most of the time, Labyrinthitis and Vestibular Neuritis will improve by themselves, with symptoms easing after a few days of rest at home and your balance returning over the next few weeks. Labyrinthitis or Vestibular Neuritis is usually caused by a viral infection, such as a cold or flu, so antibiotics will not help. However, your doctor can prescribe anti-sickness medicines to help with vertigo, nausea and vomiting. You usually only take these for a short period of time though as they may slow down your recovery.
How to manage in the first few days:
- At first, when your vertigo and sickness are at their worst, you may want to rest in bed
- When you have an attack of vertigo, it may help if you lie still and close your eyes until your symptoms go away
- Avoid changing positions or making sudden movements initially
- Avoid bright lights and loud noises
- Drink plenty of water if you’re being sick – it’s best to drink little and often
- Do not drive, cycle or use tools or machinery if you feel dizzy
- Avoid alcohol – it can make symptoms worse
- Try to get enough sleep – tiredness can make symptoms worse
- Do try to be as active as you can as soon as possible because this will help you to recover more quickly. You may want to take someone with you on a walk if you feel unsteady.
Your symptoms may come and go while you’re recovering. Labyrinthitis and Vestibular Neuritis usually clear up on their own without any complications. Your vertigo should get better within a few days. But some people continue to feel unsteady even after the initial spinning and dizziness have gone away. This can last a long time – weeks or even months. It can make you more likely to fall over.
Sometimes, Labyrinthitis can cause permanent hearing loss. It can also cause lasting damage to the balance system in your inner ear. Whether or not this happens may depend on which type of Labyrinthitis you have. This is more likely to happen if you have a bad case of Bacterial Labyrinthitis.
Vestibular rehabilitation therapy
If you’re still feeling dizzy and unsteady after a few weeks, you may benefit from vestibular rehabilitation therapy. This involves doing a range of specially designed exercises to improve your balance. It may include exercises in which you move your head or eyes, and others to improve your balance while standing or walking.
These exercises teach your brain to use the information from your eyes, joints and muscles. This helps you balance, even though there is confusing information coming from your inner ear.
Vestibular rehabilitation therapy can help with your balance and walking, and make everyday activities easier.
Here at Hallamshire Physiotherapy Clinic, our specialist Physiotherapists are trained and experienced in managing and helping you to recover from Labyrinthitis or Vestibular Neuritis.
Your treatment will be specific to you as an individual, but will usually consist of the following:
- VOR gaze stability exercises
- Postural stability exercises
- Gait re-education
- Static and dynamic balance re-training.
We will also offer our expertise, guidance and support for as long as you need us on your road to recovery.
Call us on 0114 267 1233 to book an appointment with one of our specialist clinicians.
Visual vertigo is a disorder characterised by symptoms of dizziness, vertigo, unsteadiness, disorientation, and general discomfort, caused by visual triggers. It is currently treated with vestibular rehabilitation therapy, with no effective pharmacotherapy available for treatment-resistant cases.
Symptoms typically occur during activities such as:
- Walking through busy shopping centres
- Being a passenger in a car
- Watching trains moving at a crossing
- Certain designs and patterns
- Driving past railings
- Watching action programmes on television.
Symptoms typically occur after a vestibular incident such as BPPV, vestibular neuritis/labyrinthitis or migraine.
Visual vertigo is different from ‘true’ rotational vertigo because rather than experiencing ‘rotation’ of the environment, instead the movement in the environment triggers the symptoms.
Acute vertigo usually subsides after several weeks, but occasionally you may notice lingering visual discomfort and symptom exacerbation from moving objects. This can leave you feeling frustrated and anxious about your symptoms and lack of symptom resolution.
Visual vertigo is usually because of visual dependence. There are 3 sensory systems involved in balance, your vision (eyes), vestibular system (ears) and proprioception (joints). In order to maintain balance, 2 of these systems are required to work. During visual vertigo, patients develop a dependence on their visual system.
As a result, Physiotherapy and vestibular rehabilitation is aimed at improving all aspects of the balance system and reducing the dependence on the visual fields.
If you feel you may be suffering from visual vertigo, call us on 0114 267 1233 to book an appointment with one of our specialist clinicians.
Postural phobic vertigo is when an individual suffers with dizziness and anxiety, leading to avoidance behaviour, often as a consequence of a vestibular disorder. It has been described as the most common form of dizziness in middle aged patients in dizziness units.
Anxiety disorders are common among patients with vestibular disorders. Cognitive-behavioural therapy is an effective treatment for anxiety disorders, and vestibular rehabilitation exercises are effective for vestibular disorders.
The diagnosis of postural phobic vertigo is based on 6 characteristics proposed by Brandt et al in 1996.
The diagnostic criteria are as follows:
1. Dizziness and subjective disturbance of balance while standing or walking despite normal clinical balance tests
2. Fluctuating unsteadiness for seconds to minutes, or momentary perceptions of illusory body perturbations
3. Usually a perceptual stimulus or social situation as a provoking factor with a tendency for rapid conditioning, generalization, and avoidance behaviour
4. Anxiety and vegetative symptoms during or after vertigo
5. Obsessive-compulsive personality type, labile affect, or mild depression
6. Onset frequently after a period of emotional stress, serious illness, or a vestibular disorder. Patients sometimes exhibit anxiety reactions.
We understand how disruptive and distressing vestibular conditions can be to peoples lives, both physically and mentally, and during our thorough assessment, we will look at you as a whole person and not just your condition. This way, we can truly understand the impact on your lives and how we best approach the management and treatment.
Our experienced clinicians will approach the session with empathy and understanding to make you feel as comfortable as possible and work with you to develop a strategy to regain your confidence and re-train your balance systems.
Call us on 0114 267 1233 to book an appointment with one of our specialist clinicians.
Vestibular migraine is now the internationally accepted term for a type of migraine that mainly presents with dizziness symptoms. We aim to improve the symptoms of dizziness associated with vestibular migraines and get to the root cause of the problem.
When you suffer from migraine-related dizziness, the duration of attacks is very variable, from seconds in some patients to days in others, but usually last minutes to hours. They mostly occur without headaches, although in around half of patients are followed by or occur with a headache or visual changes.
Vestibular migraine is the most common cause of recurrent spontaneous vertigo and the second most common vestibular disorder after benign paroxysmal positional vertigo (BPPV)
Common symptoms associated with a vestibular migraine are:
- Nausea
- Vomiting
- Sweating
- Flushing
- Diarrhoea
- Visual changes such as blurring, flashing lights and difficulty focusing.
Patients also report difficulty concentrating, finding bright lights and loud sounds uncomfortable and, most commonly, feel extreme tiredness and fatigue, needing to sleep.
There is a strong association with Ménière’s disease, with approximately half of people with Ménière’s experiencing at least one migraine symptom during a Ménière’s attack.
The presence of visual symptoms during attacks is not expected in Ménière’s disease and this is often the key to making the correct diagnosis.
Who does it affect?
It affects about 10% of all migraineurs. Vestibular migraine may start at any age and affects females more than males with a 3:1 ratio. There are also signs to suggest it may have a link to genetics.
Migraine in general has been shown to be closely related to anxiety and depression and the most common cause is stress! Most patients have one or more specific triggers and treatment therefore centres on identifying and managing these triggers in individual patients.
The top 5 most common triggers for vestibular migraine are;
- Stress and anxiety
- Poor sleep – both too little, and too much!
- Hunger and dehydration – missing meals and not taking enough water
- Dietary triggers – many common foods, especially caffeine and sodium (salt)
- Hormonal changes – i.e. menstruation, menopause and in teenagers.
Other external triggers can include certain forms of lighting and ventilation, weather changes, smoking and strong odours.
How is it managed?
Treatment typically revolves around education and lifestyle and dietary changes/management. This has been shown to be successful in 80-90% of patients, with medication only needed in a minimal number of patients. Vestibular rehabilitation is also useful alongside this, to help with restoring and improving the balance systems in the body.
Our specialist clinicians are experienced and knowledgeable in vestibular conditions. They will conduct a thorough assessment to understand what it is that is affecting you, before aiming to provide you with a diagnosis alongside education and vestibular rehabilitation to reduce and resolve your symptoms.
Call us on 0114 267 1223 to book an appointment with one of our specialist vestibular clinicians.
Ménière’s disease is a long term, progressive vestibular condition affecting the balance and hearing parts of the inner ear. There is no cure for Ménière’s disease but it can be managed by medications and therapy.
Ménière’s is associated with unpredictable attacks of:
- Vertigo (severe dizziness)
- Fluctuating tinnitus
- Increasing deafness
- Feeling of pressure deep within the ear.
During an attack, you may also experience:
- Unsteadiness on your feet
- Nausea and vomiting
- Ringing or buzzing inside your ear
- A sudden drop of hearing.
Symptoms vary between people and over time, but an attack of hearing loss without vertigo is uncommon. Attacks can last from a few minutes to 24 hours and can take a day or 2 for the symptoms to disappear completely. You may feel tired after an attack.
Attacks can happen in clusters, or several times a week, or they may be separated by weeks, months or years. This makes Ménière’s an unpredictable and distressing condition.
As it progresses the vertigo may be less severe; however there may be periods of imbalance, adding to the distress. In the later stages tinnitus is more prominent and fluctuating hearing loss develops. There is permanent damage to the balance organ and significant balance problems are common. Usually only one ear is affected, but up to 50% of sufferers may develop the condition in both ears.
Who does it affect?
The incidence of Ménière’s is between 1:1000 and 1:2000 of the population; depending on the source. Méniére’s can affect anyone and it can occur at any age, although most commonly affecting people between 20 and 60, being uncommon in children. About 7-10% of those affected have a family history of the condition.

What causes Ménière’s ?
The cause of Ménière’s is unknown, although it is likely that Ménière’s disease is caused by a combination of factors.
Factors that are thought to increase your risk include:
- Poor fluid drainage in your ear
- An immune system disorder
- Allergies
- A viral infection, such as meningitis
- A family history of Ménière’s disease
- A head injury
- Migraines.
Treatment for Ménière’s disease
There is no cure for Ménière’s, but treatment is aimed at reducing and controlling symptoms of vertigo, nausea and vomiting. As Ménière’s is symptomatic, treatment will vary with the needs of each individual and includes medication, vestibular rehabilitation, diet and lifestyle changes, tinnitus management, hearing aids and counselling.
In four out of five people non-surgical measures are sufficient to control the symptoms of Ménière’s; however, if vertigo remains a problem surgical procedures can help.
There are also support groups and organisations, such as the Ménière’s Society, that can provide help and advice.
What to do during an attack of Ménière’s disease
Ménière’s disease can cause you to lose balance.
At the first sign of an attack you should:
- take your vertigo medicine if you have some
- sit or lie down
- close your eyes, or keep them fixed on a still object in front of you
- do not turn your head quickly
- if you need to move, do so slowly and carefully.
Once the attack is over, try to move around to help your eyesight and other senses compensate for the problems in your inner ear.
As there is a large element of distress, alongside interference with your balance systems, specialist vestibular physiotherapists are well placed to help manage this condition through a combination of advice and education, goal-setting and management plans and vestibular rehabilitation.
Call us on 0114 267 1223 to book an appointment with one of our specialist vestibular physiotherapists to see how we can help.
Whiplash happens when your head is suddenly jolted backwards and forwards in a whip like movement. This can cause some of the muscles and ligaments in your neck to stretch. Common reasons that people get whiplash include: being involved in a car accident or having a fall.
Whiplash injury is not only limited to neck injury but also brainstem injury that does not involve direct damage to the neck or head. There are a range of whiplash symptoms with the most common complaints being neck pain, headaches and pain around the shoulder blade. Vertigo and dizziness are also reported in 25–50% of the cases.
Studies show that up to 40 per cent of people involved in car accidents, with neck trauma in the form of whiplash develop persistent symptoms.
Dizziness is one of three most common symptoms after whiplash trauma. Pain and postural unsteadiness are the other two common problems reported.
Quite often, the neck pain and stiffness that you experience can lead to altered patterns of movement that can disrupt how your balance systems interact. This can lead to dizziness or problems with your balance. This in turn can then lead to you keeping your head still to reduce the symptoms, which can lead to further pain and stiffness in your neck as you move it less.
There are also reflexes between the eyes, neck, and vestibular (inner ear) system that can be altered because of damage to the cervical spine (neck). And that brings us to the need to intervene early after neck injuries resulting in whiplash in order to prevent the transition from acute to chronic status.
Additionally, whiplash can be a traumatic experience in many ways. The accident and impact are obvious but the knock on effect can be increased fear when driving, anger and frustration from the event whether you were at fault or not, and an increase in general anxiety levels, all that can lead to protective behaviours and increased tension in the neck. This all contributes to the pain experience and can exacerbate dizzy symptoms. We are here to get you out of this vicious circle.
Physiotherapy for whiplash combines vestibular rehabilitation with treatment to the neck, to combat both of the problems simultaneously and reduce sensations of pain, stiffness and dizziness.
Call us now on 0114 267 1223 to see book an assessment with one of our experienced clinicians and reduce the impact of your injuries.
Falls can have very serious consequences as we age. Each year, more than 25 percent of adults 65 or older have a fall, and 3 million are treated in emergency departments for fall injuries, according to the Centers for Disease Control and Prevention.
The risk of falling in older adults is usually related to a combination of factors, including:
- Balance and/or walking problems. Balance can be affected by vision changes, vestibular problems and altered sensation in the feet
- The use of multiple medications. Studies indicate that when individuals take five or more medicines, the risk of falls increases
- Home hazards (including dim lighting and trip hazards)
- Positional low blood pressure (such as orthostatic hypotension, when blood pressure drops upon standing
Feet and footwear issues - Falls often occur in the bathroom when sitting or standing from the toilet or shower, or at night in a dark bedroom when getting up quickly and tripping on the way to the bathroom.
There are ways you can reduce your risk of having a fall, including making simple changes to your home and doing exercises to improve your strength and balance
If you have fallen in the past, making changes to reduce your chances of having a fall can also help you overcome any fear of falling.
If you are experiencing problems with falling, it could be related to your strength and balance, or possibly a dysfunction with your vestibular system.
Here at Hallamshire Physiotherapy Clinic, our experienced clinicians will take their time when assessing you to determine the potential causes for your falls and look to direct the most appropriate treatment to managed your problems. Quite often, there will be more than one cause for your falls and therefore our holistic approach will help to address all of these.
Strength and balance training
Doing regular strength exercises and balance exercises can improve your strength and balance and reduce your risk of having a fall.
This can take the form of simple activities such as walking and dancing, or specialist training programmes.
It’s important that a strength and balance training programme is tailored to the individual and monitored by an appropriately trained professional. We offer 1 to 1 support to ensure that our assessment and management is tailored to you as an individual.
Our partners at Community Wellness Services also offer a weekly strength and balance class directed at preventing falls in older adults, at our gym space on Ecclesall Road. Visit Community Wellness Services to find out more.
Physical activity guidelines for older adults
Older adults should do some type of physical activity every day. It can help to improve your health and reduce the risk of heart disease and stroke
The UK guidelines state that adults over 65 should:
- Aim to be physically active every day, even if it’s just light activity
- Do activities that improve strength, balance and flexibility on at least 2 days a week
- Do at least 150 minutes of moderate intensity activity a week or 75 minutes of vigorous intensity activity if you are already active, or a combination of both
- Reduce time spent sitting or lying down and break up long periods of not moving with some activity.
If you’ve fallen or are worried about falling, doing exercises to improve your strength, balance and flexibility will help make you stronger and feel more confident on your feet.
Read more about physical activity guidelines for older adults here
Call us on 0114 267 1223 to see how we may be able to help.
Cervicogenic dizziness is where you have neck pain in association with symptoms of dizziness. It is common to get neck pain along with dizziness as the body’s natural response to dizziness is to hold the head still. This however causes tension in the neck muscles and stiffness in the joints which leads to pain.
Similarly, if you have stiffness in your neck and are not moving your head normally it will create an imbalance within the balance system within the neck, which can lead to dizziness.
Rather than being stuck in this downward cycle, it is important to get to the root cause of both of the problems simultaneously, as if only one element is treated, then it is likely to return if the other remains problematic.
Symptoms
- Neck pain
- Stiffness
- Dizziness or imbalance accompanied with neck movement
- Can last several minutes to hours.
What causes Cervicogenic dizziness?
This can happen due to poor posture, osteoarthritis, rheumatoid arthritis or trauma, for example after whiplash or head injury.
Factors such as stress, lack of sleep, diet and your lifestyle can also influence your symptoms.
There are also reflexes between the eyes, neck, and vestibular (inner ear) system that can be altered following a strain on the cervical spine (neck). Physiotherapy for cervicogenic dizziness combines vestibular rehabilitation with treatment to the neck, to combat both of the problems simultaneously and reduce sensations of pain, stiffness and dizziness.
Call us on 0114 267 1223 to book an appointment with one of our experienced clinicians.
Vestibular hypofunction is when the balance part of the inner ear is not working properly. This can occur on one side (unilateral hypofunction) or on both sides (bilateral hypofunction).
Unilateral hypofunction can occur from a variety of causes:
- Vestibular neuritis
- Acoustic neuroma (non-cancerous brain tumour)
- Treatments for acoustic neuroma
- Meniere’s disease
- Treatments for Meniere’s disease.
Bilateral hypofunction can also occur from a variety of causes:
- Exposure to aminoglycoside antibiotics (which are toxic to the inner ear)
- Neurofibromatosis type II
- CANVAS syndrome (cerebellar ataxia, neuropathy, and vestibular areflexia)
- Autoimmune disease
- Congenital problems
- Trauma
- Superficial siderosis
- Idiopathic causes.
What are the symptoms?
Hypofunction of the inner ear produces symptoms related to a loss of the normal balance reflexes:
- Oscillopsia (movement or bobbing of the visual world with head movement due to loss of the vestibulo-ocular reflex)
- Dizziness
- Postural instability.
- Visual Vertigo
- Cognitive deficits such as fatigue or ‘brain fog’.
Treatment
Both unilateral and bilateral vestibular hypofunction are treated with vestibular rehabilitation.
In unilateral hypofunction, treatment is aimed at promoting central compensation and relies on the other ear (the normal side) to perform most of the inner ear functions.
In bilateral hypofunction, vestibular rehabilitation can still be helpful, but therapy is often longer and more difficult, as the absence of all inner ear function means that you have to rely on other systems (such as the COR- cervical-ocular reflex) to sense head movements.
Here at Hallamshire Physiotherapy clinic, our specialist therapists are experienced in vestibular conditions and can help with advice and education as well as vestibular rehabilitation. We can also direct you to an appropriate consultant if we feel that their expertise is also required in your management.
Vestibular Neuritis is an infection of the vestibular nerve within the inner ear. Labyrinthitis is an infection of the inner ear, specifically the labyrinth.
Your inner ear is made up of a system of fluid-filled tubes called the labyrinth. This includes your cochlea, which senses sound, and your vestibular system, which senses movement of your head and helps with balance. Your vestibular nerve passes through your inner ear, taking messages to your brain.
Symptoms
Symptoms can start suddenly and can be associated with flu-like symptoms such as a sore throat, runny nose or a fever.
The symptoms of Vestibular Neuritis are very similar to Labyrinthitis, though it does not cause hearing loss or tinnitis.
- Dizziness or spinning sensations (Vertigo)
- Unsteadiness and feeling off balance
- Nausea and vomiting.
Labyrinthitis and Vestibular Neuritis can affect both adults and children, but they’re most common between the ages of 30 and 60.

Causes
There are various causes for Vestibular Neuritis and Labyrinthitis.
In the majority of cases, they are caused by a viral infection. However, in rarer cases it can be as a result of the following:
- Bacterial infections, usually middle ear infection (otitis media) or meningitis, that spread to your inner ear. These are more common in children than in adults
- Autoimmune conditions affecting your inner ear. This is a less common cause. If you have an autoimmune condition, your immune system mistakenly attacks some of your body’s healthy tissues, causing inflammation and damage
- Damage to your inner ear, due to an underlying disease, such as meningitis, circulatory problems or Ménière’s disease.
How are they treated?
Most of the time, Vestibular Neuritis and Labyrinthitis will improve by themselves, with symptoms easing after a few days of rest at home and your balance returning over the next few weeks. Vestibular Neuritis or Labyrinthitis is usually caused by a viral infection, such as a cold or flu, so antibiotics will not help. However, your doctor can prescribe anti-sickness medicines to help with vertigo, nausea and vomiting. You usually only take these for a short period of time though as they may slow down your recovery.
How to manage in the first few days:
- At first, when your vertigo and sickness are at their worst, you may want to rest in bed
- When you have an attack of vertigo, it may help if you lie still and close your eyes until your symptoms go away
- Avoid changing positions or making sudden movements initially
- Avoid bright lights and loud noises
- Drink plenty of water if you’re being sick – it’s best to drink little and often
- Do not drive, cycle or use tools or machinery if you feel dizzy
- Avoid alcohol – it can make symptoms worse
- Try to get enough sleep – tiredness can make symptoms worse
- Do try to be as active as you can as soon as possible because this will help you to recover more quickly. You may want to take someone with you on a walk if you feel unsteady.
Your symptoms may come and go while you’re recovering. Vestibular Neuritis and Labyrinthitis usually clear up on their own without any complications. Your vertigo should get better within a few days. But some people continue to feel unsteady even after the initial spinning and dizziness have gone away. This can last a long time – weeks or even months. It can make you more likely to fall over.
Vestibular rehabilitation therapy
If you’re still feeling dizzy and unsteady after a few weeks, you may benefit from vestibular rehabilitation therapy. This involves doing a range of specially designed exercises to improve your balance. It may include exercises in which you move your head or eyes, and others to improve your balance while standing or walking.
These exercises teach your brain to use the information from your eyes, joints and muscles. This helps you balance, even though there is confusing information coming from your inner ear.
Vestibular rehabilitation therapy can help with your balance and walking, and make everyday activities easier.
Here at Hallamshire Physiotherapy Clinic, our specialist Physiotherapists are trained and experienced in managing and helping you to recover from Vestibular Neuritis or Labyrinthitis.
Your treatment will be specific to you as an individual, but will usually consist of the following:
- VOR gaze stability exercises
- Postural stability exercises
- Gait re-education
- Static and dynamic balance re-training.
We will also offer our expertise, guidance and support for as long as you need us on your road to recovery.
Call us on 0114 267 1233 to book an appointment with one of our specialist clinicians.